Archive for May, 2014
A Wash On the Wild Side: How I Learned To Stop Worrying and Love My Microbiome
Sunday, May 25th, 2014
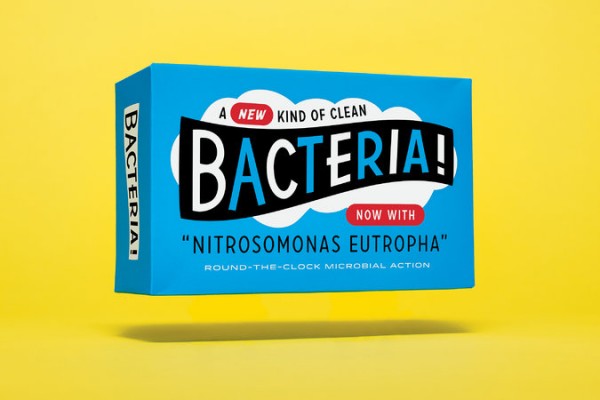
For most of my life, if Iâve thought at all about the bacteria living on my skin, it has been while trying to scrub them away. But recently I spent four weeks rubbing them in. I was Subject 26 in testing a living bacterial skin tonic, developed by AOBiome, a biotech start-up in Cambridge, Mass. The tonic looks, feels and tastes like water, but each spray bottle of AO+ Refreshing Cosmetic Mist contains billions of cultivated Nitrosomonas eutropha, an ammonia-oxidizing bacteria (AOB) that is most commonly found in dirt and untreated water. AOBiome scientists hypothesize that it once lived happily on us too â before we started washing it away with soap and shampoo â acting as a built-in cleanser, deodorant, anti-inflammatory and immune booster by feeding on the ammonia in our sweat and converting it into nitrite and nitric oxide.
In the conference room of the cramped offices that the four-person AOBiome team rents at a start-up incubator, Spiros Jamas, the chief executive, handed me a chilled bottle of the solution from the refrigerator. âThese are AOB,â he said. âTheyâre very innocuous.â Because the N. eutropha are alive, he said, they would need to be kept cold to remain stable. I would be required to mist my face, scalp and body with bacteria twice a day. I would be swabbed every week at a lab, and the samples would be analyzed to detect changes in my invisible microbial community.
In the last few years, the microbiome (sometimes referred to as âthe second genomeâ) has become a focus for the health conscious and for scientists alike. Studies like the Human Microbiome Project, a national enterprise to sequence bacterial DNA taken from 242 healthy Americans, have tagged 19 of our phyla (groupings of bacteria), each with thousands of distinct species. As Michael Pollan wrote in this magazine last year: âAs a civilization, weâve just spent the better part of a century doing our unwitting best to wreck the human-associated microbiota. . . . Whether any cures emerge from the exploration of the second genome, the implications of what has already been learned â for our sense of self, for our definition of health and for our attitude toward bacteria in general â are difficult to overstate.â
While most microbiome studies have focused on the health implications of whatâs found deep in the gut, companies like AOBiome are interested in how we can manipulate the hidden universe of organisms (bacteria, viruses and fungi) teeming throughout our glands, hair follicles and epidermis. They see long-term medical possibilities in the idea of adding skin bacteria instead of vanquishing them with antibacterials â the potential to change how we diagnose and treat serious skin ailments. But drug treatments require the approval of the Food and Drug Administration, an onerous and expensive process that can take upward of a decade. Instead, AOBiomeâs founders introduced AO+ under the loosely regulated âcosmeticsâ umbrella as a way to release their skin tonic quickly. With luck, the sales revenue will help to finance their research into drug applications. âThe cosmetic route is the quickest,â Jamas said. âThe other route is the hardest, the most expensive and the most rewarding.â
AOBiome does not market its product as an alternative to conventional cleansers, but it notes that some regular users may find themselves less reliant on soaps, moisturizers and deodorants after as little as a month. Jamas, a quiet, serial entrepreneur with a doctorate in biotechnology, incorporated N. eutropha into his hygiene routine years ago; today he uses soap just twice a week. The chairman of the companyâs board of directors, Jamie Heywood, lathers up once or twice a month and shampoos just three times a year. The most extreme case is David Whitlock, the M.I.T.-trained chemical engineer who invented AO+. He has not showered for the past 12 years. He occasionally takes a sponge bath to wash away grime but trusts his skinâs bacterial colony to do the rest. I met these men. I got close enough to shake their hands, engage in casual conversation and note that they in no way conveyed a sense of being âuncleanâ in either the visual or olfactory sense.
For my part in the AO+ study, I wanted to see what the bacteria could do quickly, and I wanted to cut down on variables, so I decided to sacrifice my own soaps, shampoo and deodorant while participating. I was determined to grow a garden of my own.
Week One
The story of AOBiome begins in 2001, in a patch of dirt on the floor of a Boston-area horse stable, where Whitlock was collecting soil samples. A few months before, an equestrienne he was dating asked him to answer a question she had long been curious about: Why did her horse like to roll in the dirt? Whitlock didnât know, but he saw an opportunity to impress.
Whitlock thought about how much horses sweat in the summer. He wondered whether the animals managed their sweat by engaging in dirt bathing. Could there be a kind of âgoodâ bacteria in the dirt that fed off perspiration? He knew there was a class of bacteria that derive their energy from ammonia rather than from carbon and grew convinced that horses (and possibly other mammals that engage in dirt bathing) would be covered in them. âThe only way that horses could evolve this behavior was if they had substantial evolutionary benefits from it,â he told me.
Whitlock gathered his samples and brought them back to his makeshift home laboratory, where he skimmed off the dirt and grew the bacteria in an ammonia solution (to simulate sweat). The strain that emerged as the hardiest was indeed an ammonia oxidizer: N. eutropha. Here was one way to test his âclean dirtâ theory: Whitlock put the bacteria in water and dumped them onto his head and body.
Some skin bacteria species double every 20 minutes; ammonia-oxidizing bacteria are much slower, doubling only every 10 hours. They are delicate creatures, so Whitlock decided to avoid showering to simulate a pre-soap living condition. âI wasnât sure what would happen,â he said, âbut I knew it would be good.â
The bacteria thrived on Whitlock. AO+ was created using bacterial cultures from his skin.
And now the bacteria were on my skin.
I had warned my friends and co-workers about my experiment, and while there were plenty of jokes â someone left a stick of deodorant on my desk; people started referring to me as âTeen Spiritâ â when I pressed them to sniff me after a few soap-free days, no one could detect a difference. Aside from my increasingly greasy hair, the real changes were invisible. By the end of the week, Jamas was happy to see test results that showed the N. eutropha had begun to settle in, finding a friendly niche within my biome.
Week Two
AOBiome is not the first company to try to leverage emerging discoveries about the skin microbiome into topical products. The skin-care aisle at my drugstore had a moisturizer with a âprobiotic complex,â which contains an extract of Lactobacillus, species unknown. Online, companies offer face masks, creams and cleansers, capitalizing on the booming market in probiotic yogurts and nutritional supplements. There is even a âfrozen yogurtâ body cleanser whose second ingredient is sodium lauryl sulfate, a potent detergent, so you can remove your healthy bacteria just as fast as you can grow them.
Audrey Gueniche, a project director in LâOrĂ©alâs research and innovation division, said the recent skin microbiome craze âhas revolutionized the way we study the skin and the results we look for.â LâOrĂ©al has patented several bacterial treatments for dry and sensitive skin, including Bifidobacterium longum extract, which it uses in a LancĂŽme product. Clinique sells a foundation with Lactobacillus ferment, and its parent company, EstĂ©e Lauder, holds a patent for skin application of Lactobacillus plantarum. But itâs unclear whether the probiotics in any of these products would actually have any effect on skin: Although a few studies have shown that Lactobacillus may reduce symptoms of eczema when taken orally, it does not live on the skin with any abundance, making it âa curious place to start for a skin probiotic,â said Michael Fischbach, a microbiologist at the University of California, San Francisco. Extracts are not alive, so they wonât be colonizing anything.
To differentiate their product from others on the market, the makers of AO+ use the term âprobioticsâ sparingly, preferring instead to refer to âmicrobiomics.â No matter what their marketing approach, at this stage the company is still in the process of defining itself. It doesnât help that the F.D.A. has no regulatory definition for âprobioticâ and has never approved such a product for therapeutic use. âThe skin microbiome is the wild frontier,â Fischbach told me. âWe know very little about what goes wrong when things go wrong and whether fixing the bacterial community is going to fix any real problems.â
I didnât really grasp how much was yet unknown until I received my skin swab results from Week 2. My overall bacterial landscape was consistent with the majority of Americansâ: Most of my bacteria fell into the genera Propionibacterium, Corynebacterium and Staphylococcus, which are among the most common groups. (S. epidermidis is one of several Staphylococcus species that reside on the skin without harming it.) But my test results also showed hundreds of unknown bacterial strains that simply havenât been classified yet.
Meanwhile, I began to regret my decision to use AO+ as a replacement for soap and shampoo. People began asking if Iâd âdone something newâ with my hair, which turned a full shade darker for being coated in oil that my scalp wouldnât stop producing. I slept with a towel over my pillow and found myself avoiding parties and public events. Mortified by my body odor, I kept my arms pinned to my sides, unless someone volunteered to smell my armpit. One friend detected the smell of onions. Another caught a whiff of âpleasant pot.â
When I visited the gym, I followed AOBiomeâs instructions, misting myself before leaving the house and again when I came home. The results: After letting the spray dry on my skin, I smelled better. Not odorless, but not as bad as I would have ordinarily. And, oddly, my feet didnât smell at all.
Week Three
My skin began to change for the better. It actually became softer and smoother, rather than dry and flaky, as though a saunaâs worth of humidity had penetrated my winter-hardened shell. And my complexion, prone to hormone-related breakouts, was clear. For the first time ever, my pores seemed to shrink. As I took my morning âshowerâ â a three-minute rinse in a bathroom devoid of hygiene products â I remembered all the antibiotics I took as a teenager to quell my acne. How funny it would be if adding bacteria were the answer all along.
Dr. Elizabeth Grice, an assistant professor of dermatology at the University of Pennsylvania who studies the role of microbiota in wound healing and inflammatory skin disease, said she believed that discoveries about the second genome might one day not only revolutionize treatments for acne but also â as AOBiome and its biotech peers hope â help us diagnose and cure disease, heal severe lesions and more. Those with wounds that fail to respond to antibiotics could receive a probiotic cocktail adapted to fight the specific strain of infecting bacteria. Body odor could be altered to repel insects and thereby fight malaria and dengue fever. And eczema and other chronic inflammatory disorders could be ameliorated.
According to Julie Segre, a senior investigator at the National Human Genome Research Institute and a specialist on the skin microbiome, there is a strong correlation between eczema flare-ups and the colonization of Staphylococcus aureus on the skin. Segre told me that scientists donât know what triggers the bacterial bloom. But if an eczema patient could monitor their microbes in real time, they could lessen flare-ups. âJust like someone who has diabetes is checking their blood-sugar levels, a kid who had eczema would be checking their microbial-diversity levels by swabbing their skin,â Segre said.
AOBiome says its early research seems to hold promise. In-house lab results show that AOB activates enough acidified nitrite to diminish the dangerous methicillin-resistant Staphylococcus aureus (MRSA). A regime of concentrated AO+ caused a hundredfold decrease of Propionibacterium acnes, often blamed for acne breakouts. And the company says that diabetic mice with skin wounds heal more quickly after two weeks of treatment with a formulation of AOB.
Soon, AOBiome will file an Investigational New Drug Application with the F.D.A. to request permission to test more concentrated forms of AOB for the treatment of diabetic ulcers and other dermatologic conditions. âItâs very, very easy to make a quack therapy; to put together a bunch of biological links to convince someone that somethingâs true,â Heywood said. âWhat would hurt us is trying to sell anything ahead of the data.â
Week Four
As my experiment drew to a close, I found myself reluctant to return to my old routine of daily shampooing and face treatments. A month earlier, I packed all my hygiene products into a cooler and hid it away. On the last day of the experiment, I opened it up, wrinkling my nose at the chemical odor. Almost everything in the cooler was a synthesized liquid surfactant, with lab-manufactured ingredients engineered to smell good and add moisture to replace the oils they washed away. I asked AOBiome which of my products was the biggest threat to the âgoodâ bacteria on my skin. The answer was equivocal: Sodium lauryl sulfate, the first ingredient in many shampoos, may be the deadliest to N. eutropha, but nearly all common liquid cleansers remove at least some of the bacteria. Antibacterial soaps are most likely the worst culprits, but even soaps made with only vegetable oils or animal fats strip the skin of AOB.
Bar soaps donât need bacteria-killing preservatives the way liquid soaps do, but they are more concentrated and more alkaline, whereas liquid soaps are often milder and closer to the natural pH of skin. Which is better for our bacteria? âThe short answer is, we donât know,â said Dr. Larry Weiss, founder of CleanWell, a botanical-cleanser manufacturer. Weiss is helping AOBiome put together a list of âbacteria-safeâ cleansers based on lab testing. In the end, I tipped most of my products into the trash and purchased a basic soap and a fragrance-free shampoo with a short list of easily pronounceable ingredients. Then I enjoyed a very long shower, hoping my robust biofilm would hang on tight.
One week after the end of the experiment, though, a final skin swab found almost no evidence of N. eutropha anywhere on my skin. It had taken me a month to coax a new colony of bacteria onto my body. It took me three showers to extirpate it. Billions of bacteria, and they had disappeared as invisibly as they arrived. I had come to think of them as âmine,â and yet I had evicted them.
– – –
BONUS: Eavesdrop on Julia’s conversation with The 6th Floor blog at the New York Times.
Tags: AOBiome, Bacteria, Bacteria skin spray, Julia Scott, Julie Segre, Lactobacillus, Michael Fischbach, New York Times Magazine, Nitrosomonas Eutropha, No poo, Probiotic cleanser, Probiotic cosmetics, Probiotic FDA regulation, Probiotics, Skin microbiome, Sodium laurel sulfate
Posted in Feature | No Comments »
© 2024 Julia Scott.